Medical Front Desk Receptionist (Bilingual - Spanish Required) - 180 Degrees Medical PLLC: Wound Care, Weight Loss, and Aesthetics
8 July 2025•682 views
Expires in 15 days




We are looking for a professional, reliable, and experienced Medical Front Desk Receptionist to join our healthcare team. The ideal candidate must be fluent in Spanish and English and have proven experience with insurance verification, patient eligibility checks, and prior authorizations. This position is essential in ensuring a smooth patient flow and excellent customer service experience for our diverse patient population.
Key Responsibilities:
Greet patients warmly, check patients in and out, and manage patient intake forms.
Answer multi-line phones, schedule and confirm appointments, and handle patient inquiries professionally.
Verify patient insurance coverage, obtain authorizations, and check eligibility prior to appointments.
Process prior authorizations for medications, procedures, and diagnostic tests.
Order patient supplies.
Manage patient referral.
Collect co-pays and patient balances; post payments accurately.
Assist with maintaining accurate patient records and updating demographic information.
Serve as an interpreter for Spanish-speaking patients as needed.
Ensure patient confidentiality and compliance with HIPAA regulations.
Support providers and clinical staff with administrative tasks as needed.
Qualifications:
High school diploma or equivalent required.
Fluent in Spanish and English (speaking, reading, and writing) — required.
Minimum 1–2 years of experience as a medical front desk receptionist or medical office assistant.
Strong knowledge of insurance plans, eligibility, and prior authorization processes.
Familiarity with Electronic Medical Records (EMR) systems (e.g., eClinicalWorks, Athena, Epic).
Excellent communication and customer service skills.
Ability to multitask and remain organized in a busy medical office environment.
Professional appearance and demeanor.
Company Description
We are a patient centered physician's office that provides Internal Medicine, Obesity Medicine, and Aesthetic Care services. We are Looking to expand our team!
Company Description
We are a patient centered physician's office that provides Internal Medicine, Obesity Medicine, and Aesthetic Care services. We are Looking to expand our team!
- Experience
- Required
- Languages
- English – Beginner
Spanish – Beginner
- Employment
- Full-time
227 East 105th Street, Manhattan, 10029, New York

Medical Office • 1-10 Employees
Hiring on JOB TODAY since August, 2023
New office with 1 provider.



Post a job and hire
Similar jobs
- private concierge services
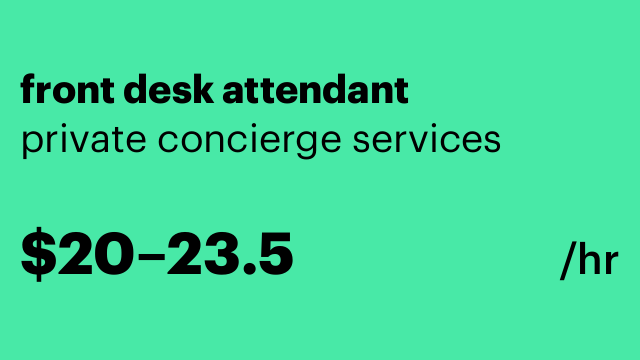 front desk attendant4 days ago$20–$23.5 hourlyFull-timeManhattan, New York
front desk attendant4 days ago$20–$23.5 hourlyFull-timeManhattan, New YorkWe are looking for candidates for our luxury condominiums and complexes. We strive to provide the best people for our clients needs in some of their most prestigious buildings! Duties will include but are not limited to: Meeting, greeting and directing residents and guests. Verifying and recording visitor information. Answering calls professionally and assists callers with directions or instructions for the building. Receive and process incoming mail/packages. Monitor lobby traffic and alert residents to arriving guests and deliveries. Maintain logbooks for visitors and contractors Qualifications: Proven customer service experience Detail oriented Professionalism Friendly/outgoing and personable Basic computer and typing skills-
Easy apply - SERGIU MARCUS, MD, PC
 Part Time Medical Assistant25 days agoPart-timeManhattan, New York
Part Time Medical Assistant25 days agoPart-timeManhattan, New YorkWe are seeking a dedicated and skilled Medical Assistant to join our healthcare team. The ideal candidate will play a crucial role in supporting our medical staff and ensuring high-quality patient care. This position requires a blend of clinical and administrative skills, with a focus on delivering exceptional patient service in a fast-paced environment. Duties Assist healthcare providers with patient examinations and procedures, ensuring comfort and safety. Perform intake procedures, including taking vital signs and documenting medical histories. Administer medications as directed and assist with basic life support when necessary. Manage electronic health records (EHR) systems to maintain accurate patient information. Support medical administrative tasks such as scheduling appointments, managing patient flow, and handling medical terminology. Conduct X-ray procedures as needed and assist in outpatient and inpatient settings. Collaborate with interdisciplinary teams in various specialties, including dermatology, urgent care, internal medicine, geriatrics, emergency medicine, and hospital medicine. Ensure compliance with ICD coding standards for accurate billing and insurance processing. Provide compassionate patient care while maintaining confidentiality and adhering to healthcare regulations. Requirements Proven experience as a Medical Assistant or in a similar role within a clinical setting. Knowledge of anatomy, physiology, medical terminology, and basic life support techniques. Familiarity with EHR systems and ability to perform administrative tasks efficiently. Experience in various medical environments such as clinics, hospitals (Level I & II trauma centers), PICU, OR, or medical-surgical units is preferred. Strong communication skills with the ability to provide excellent patient service. Ability to work collaboratively within a team while managing multiple priorities effectively. Bilingual English/Spanish Job Type: Part-time Pay: $20.00 - $26.00 per hour Expected hours: 12 per week Medical Specialty: Ophthalmology Work Location: In person
Easy apply - Mighty Minds and Muscles Therapy & Coaching Services - Padra Smith, MS, OTR/L
 Healthcare Administrative Coordinator1 month ago$25–$40 hourlyFull-timeManhattan, New York
Healthcare Administrative Coordinator1 month ago$25–$40 hourlyFull-timeManhattan, New YorkWe are a growing pediatric therapy clinic located in the heart of New York City, dedicated to providing high-quality occupational, physical, and speech therapy to children and families. Our compassionate, multidisciplinary team is committed to delivering client-centered care in a supportive and inclusive environment. Position Summary We are seeking a detail-oriented, organized, and proactive Healthcare Administrative Coordinator to support day-to-day clinic operations, with significant responsibility for billing, insurance verification, and revenue cycle management. This role begins as a contractor position, with a path to permanent employment based on performance and clinic needs. Key Responsibilities Billing & Insurance (60%) Manage end-to-end billing processes for private clients and third-party insurance payers. Verify insurance eligibility and benefits prior to services rendered. Submit and track claims through clearinghouses or EMR systems. Follow up on unpaid claims, denials, and appeals to ensure timely reimbursements. Generate patient statements and manage patient billing inquiries professionally and empathetically. Administrative Support (40%) Assist in scheduling appointments and managing clinician calendars. Maintain up-to-date client records and intake documentation in EMR. Ensure HIPAA compliance across all administrative processes. Support general clinic operations, including supply ordering, front desk coverage, and coordination with therapists and families. Qualifications Associate’s or Bachelor’s degree in Healthcare Administration, Business, or related field (or equivalent experience). Minimum 2 years of experience in a healthcare administrative role, ideally in a pediatric or therapy clinic. Hands-on experience with insurance billing, including knowledge of CPT codes, ICD-10, EOBs, and appeals. Familiarity with EMR systems and billing platforms (e.g., Fusion, Therabill, SimplePractice, Ocean Friends, or similar). Excellent communication and interpersonal skills, especially with families of pediatric clients. Strong attention to detail and organizational skills. Ability to work independently and handle sensitive information with confidentiality. To Apply Please submit your resume and a brief cover letter outlining your relevant experience in healthcare administration and billing. Candidates currently located in NYC or with plans to relocate are strongly preferred.
Easy apply - Building Service 32BJ Benefit Funds
 Customer Service Representative (CSR)2 months ago$50926.57–$53063.84 yearlyFull-timeManhattan, New York
Customer Service Representative (CSR)2 months ago$50926.57–$53063.84 yearlyFull-timeManhattan, New YorkJob Title: Member Services Representative (Benefits Specialist) Department: Member Services The 32BJ Benefit Funds is growing, and we’re currently seeking mission-driven Benefit Specialists (Member Services Representatives) to join our team. We offer: Competitive Salary coupled with a great work/life balance Prime Location - Flatiron District in Manhattan (NYC) Comprehensive Health Package including medical, dental & vision coverage with no employee contribution to the premium for a family plan Pension Benefit that includes monthly employer contributions Retirement Benefit that includes 3% 401K employer contributions Professional Coverage/Reimbursement includes Tuition Reimbursement Program Paid Time Off including vacation, personal, and sick days Federal Paid Holidays – Up to 11 days off with pay And more... Mission-driven, internal job growth opportunities Annual Salary Clarification: Non-Bilingual: $50,926.57; Bilingual: $53,063.84 - Per Collective Bargaining Agreement (CBA) FLSA Status: Non-Exempt (Eligible for OT per business needs) Work Hours: 35 Total (Available shifts Monday-Friday 8:30am-6:00pm) About Us: Building Services 32BJ Benefit Funds (“the Funds”) is the umbrella organization responsible for administering Health, Pension, Retirement Savings, Training, and Legal Services benefits to over 100,000 SEIU 32BJ members. Our mission is to make significant contributions to the lives of our members by providing high quality benefits and services. Through our commitment, we embody five core values: Flexibility, Initiative, Respect, Sustainability, and Teamwork (FIRST). By following our core values, employees are open to different and new ways of doing things, take active steps to improve the organization, create an environment of trust and respect, approach their work with the intent of a positive outcome, and work collaboratively with colleagues. For 2023 and beyond, 32BJ Benefit Funds will continue to drive innovation, equity, and technology insights to further help the lives of our hard-working members and their families. We use cutting edge technology such as: M365, Dynamics 365 CRM, Dynamics 365 F&O, Azure, AWS, SQL, Snowflake, QlikView, and more. Through this technology investment, we have gathered and analyzed thousands of data insights to influence health insurance legislation and propose new health policy. Our efforts have galvanized many leaders and the consensus is there is plenty more work to be done. Please take a moment to watch our video to learn more about our culture and contributions to our members: youtu.be/hYNdMGLn19A Position Summary: After extensive paid training and under the supervision of the Member Services Call Center or Welcome Center Supervisor and MSR 2/3 Team, works as a Benefits Specialist for the Member Services Call Center or Welcome Center to assist participants with information for all the benefits offered by the Fund. Essential Duties and Responsibilities: Collecting and analyzing data/information to resolve a problem in real time, at high volume standards. Provide customer service to participants to resolve eligibility or Fund benefit issues. Displayed proficiency in all processing systems: eligibility process, Health benefits and system, COOL/V3/DYNAMICS system, CRM/WF and vendor systems Displayed proficiency in all Funds (Health, Pension, Legal, SRSP, Shortman). Handling of inquiries through vendors, Medical, Optical, Pharmacy, Dental and Employee Assistance. Follow workflows to resolve participant questions. Representatives analyze and interpret customer phone and written correspondence. Ongoing management of own inventory of work accumulated through Participant interactions/inquiries. These inquiries will involve customer complaints or inquiries on eligibility, enrollment, benefits and claims, and Pension related issues. Operating computers with multiple information screens to research and resolve customer inquiries on line. Representatives ensure that all processing meets or exceeds MSR Quality measurement objective and performance standards, including, but not limited to, handling and documentation. Ability to effectively communicate to Participants. Perform any other relevant, related or pertinent work or duties as requested or assigned. Qualifications: To perform the job satisfactorily, an individual must be able to perform each essential duty satisfactorily. The requirements listed below are representative of the knowledge, skill, and/or ability required. As well, the candidate must be free of any disciplinary actions. Technical Skills: Strong computer skills. Detailed knowledge of benefits as displayed in training and determined through subject matter exams utilizing OneView, vendor systems, COOL/V3/DYNAMICS and CRM processing system. Ability to prioritize work and meet deadlines. A demonstrated capability to manipulate and use multiple software programs and macros simultaneously including Excel, Microsoft Word, Windows and Outlook applications. Strong analytical, problem solving and decision-making skills. Excellent organizational and prioritizing skills. Strong ability to multitask. Various work schedules available. Interpersonal Skills: Strong oral and written interpersonal skills. Demonstrated customer service orientation. Ability to effectively operate in fast-paced work environment. Excellent listening skills. Detail oriented with excellent organization and communication skills. Experience working directly with customers. Education and/or Experience: High School diploma, some college preferred; Health Care, Employee Benefits and/or Customer Service experience are strongly preferred. Bilingual Language Skills: Fluent in multiple languages is a plus, but not required. Reasoning Ability: Above average. Certificates, Licenses, Registrations: None
Immediate start!No experienceEasy apply